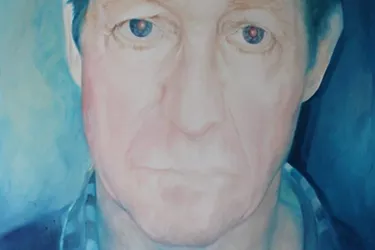
The view from the other side: a GP’s experience
Cardiff GP Chris talks about what it’s like to treat a patient with a mental health problem against a backdrop of staff shortages and increasing demand.
Chris is a salaried GP in Cardiff with an interest in improving local services. He tweets at @cbryant85
You can picture the scene. A waiting room crowded with chairs, nearly all of them taken. A true cross-section of the local population - the elderly jammed in next to young mothers, crying children and people that look mysteriously uncomfortable. I walk in and all the faces turn towards me expectantly. I call a name that I didn’t know ten minutes before and someone stands up, looking worried, tears in their eyes. The consultation has already begun, and I’m the doctor.
What follows is an emotional journey for both of us. In what was supposed to be a 10-minute appointment (predictably, it isn’t), we introduce ourselves, size each other up and try to make things better.
"I see a person struggling to wrangle a lifetime’s worth of emotion into words and get this across to a total stranger."
I see a person struggling to wrangle a lifetime’s worth of emotion into words and get this across to a total stranger. I can see they’re conflicted about how much they should say – perhaps because they feel guilty about it, perhaps because they don’t want to seem ‘crazy’, or perhaps because, lets face it, we’re British and anything beyond discussing the weather is getting a bit much.
I hope that they see me as calm and warm and someone that they can talk to, if not because they like me then at least because it’s my job to listen. They talk, I talk. I talk a lot. I try to rein it in, give them space and try not to fill the silence.
I’ll be honest, a part of my brain is aware that I’m getting further behind, that I’m keeping everyone waiting, that I won’t have time to do the paperwork I need to do. I tell that part of my brain to be quiet; my priority is the person in front of me right now, and I know this consultation will shape our relationship.
"I try to come across as positive, but I dread what’s coming next - there’s no easy fix, no magic pill."
Having opened up and broken down, they’re looking pretty exhausted and raw now, but they’re also looking to me for answers. I try to come across as positive, but I dread what’s coming next - there’s no easy fix, no magic pill. What comes next is a journey and neither of us knows where it’s going. I can make an educated guess that there’s going to be ups and downs.
We talk about counselling and agree that it sounds like a good idea, although having painted a picture of it as the best thing ever, I’m sure that I can’t help but wince as I tell them it’ll probably be at least a six week wait. I feel powerless, guilty, like I’m letting them down. We talk about other things that might help. I have a love-hate relationship with antidepressant medication and I try to get across a realistic understanding of it. We agree to stick that idea on the shelf for now.
Time off work is arguably a double-edged sword, and as anyone who’s lived on Statutory Sick Pay for a while will know, it’s not a holiday. Still, I think it might help them have some space to think, get some sleep and disentangle their problems from the big black cloud over them. We haggle over the time off; from my experience a week is never enough, but a month makes them feel like they’re kissing their career goodbye. We settle on two weeks.
"We’re busy, we’re understaffed, we don’t have enough appointments; I know it’s not OK."
I book them a follow up appointment myself, knowing that they’d struggle otherwise. We’re busy, we’re understaffed, we don’t have enough appointments; I know it’s not OK. I try to reassure them that if they need help they can speak to me sooner and I’ll “slot them in”, knowing that often people put off seeing their GP because it’s too much hassle to book an appointment.
If I think about it too much it starts to feel like I’m treading water and the waves of increasing demand are coming faster than I can do anything about. I know that it’s people with mental health problems that are amongst the hardest hit because mental health problems aren’t predictable. There will be dark times, and these times are when they will need someone the most. Not being able to offer them an appointment that day is kicking them when they are down.
The consultation ends and they leave the room. I try to make some notes that will help me write my referral for counselling later on. A few sentences doesn’t really do it justice, but I need to convey a diagnosis, an assessment of risk and a plan in case someone else has to take up from where I left off. Seeing it written down makes it seem like nothing happened in that consultation. Maybe it didn’t, but it was definitely the start of the journey.
I try to clear my head and look at the next name on my list for this morning. Another name I don’t know, and another apology for running late.
"Looking back, it seems wrong that my training so lacked emphasis on mental health."
The further I progress in my career, the more I have come to realise that physical health, mental health and wellbeing are inextricably linked. Looking back, it seems wrong that my training so lacked emphasis on mental health.
Working as a GP, I have new patients coming in daily specifically seeking help for mental health problems. Often it can feel like an impossible task to help someone within the confines of a ten-minute appointment. It’s even harder when you know what might help but you’re restricted in what you can offer.
I don’t have specific training in counselling, yet often I feel that I have to ‘plug the gap’ as there is a waiting list for everything apart from seeing me.
Primary care has never been more pushed. With a constantly increasing workload, I’m sure I’m not alone in worrying that I’ll miss an opportunity to intervene when it might be critical.
Worries like this sap our job satisfaction and push us towards our own mental health problems. We need a greater emphasis on promoting good mental health both for our patients and ourselves.
"Part of being a GP is taking on peoples problems and making them your own, even if for just ten minutes."
It all sounds bleak, but I really do love my job. The opportunity to get to know people and be let in on a significant part of their life is a privilege. Part of being a GP is taking on peoples problems and making them your own, even if for just ten minutes.
Downs are inevitable, and they take their toll. However, the ups can be magnificent and the sense that you had some small part in that brings enormous satisfaction.

Information and support
When you’re living with a mental health problem, or supporting someone who is, having access to the right information - about a condition, treatment options, or practical issues - is vital. Visit our information pages to find out more.
Share your story with others
Blogs and stories can show that people with mental health problems are cared about, understood and listened to. We can use it to challenge the status quo and change attitudes.